The American Cancer Society already has estimates for Cervical Cancer in 2023, and research reveals that around 13,960 new cases of invasive cervical cancer will be detected, with approximately 4,310 women dying from the disease.
This estimate is entirely based on the United States. When we look at the figures worldwide, it becomes more alarming; an estimated 604,127 women were diagnosed with cervical cancer in 2020.
As we all know, knowledge is power, and the purpose of this article is to provide you with all of the information for better understanding cervical cancer, including its causes, treatments, and, most importantly, whether it is preventable.
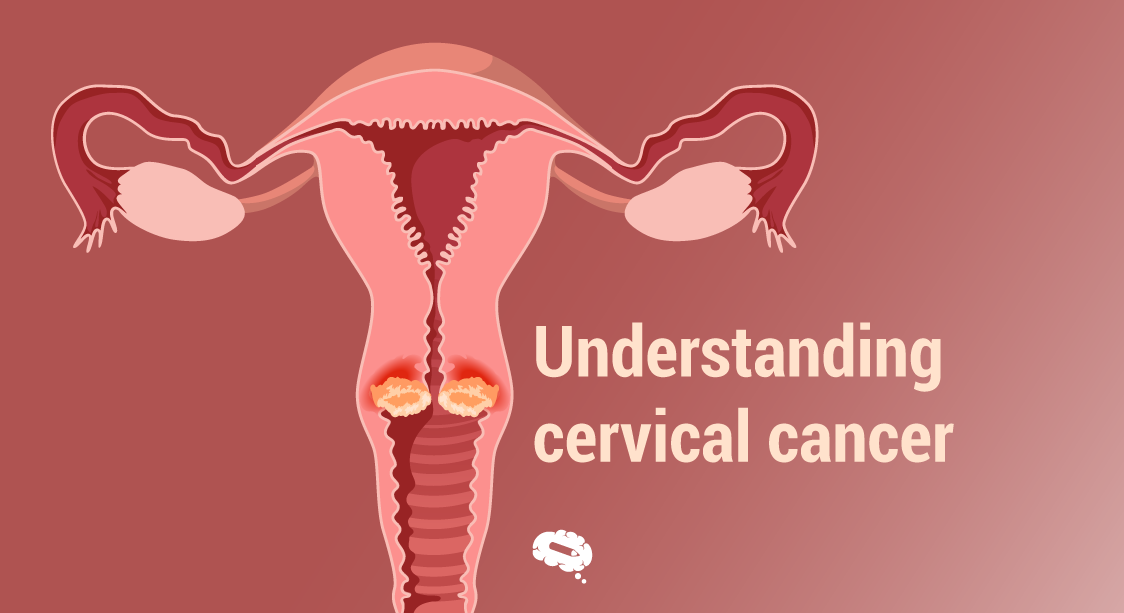
Understanding Cervical Cancer
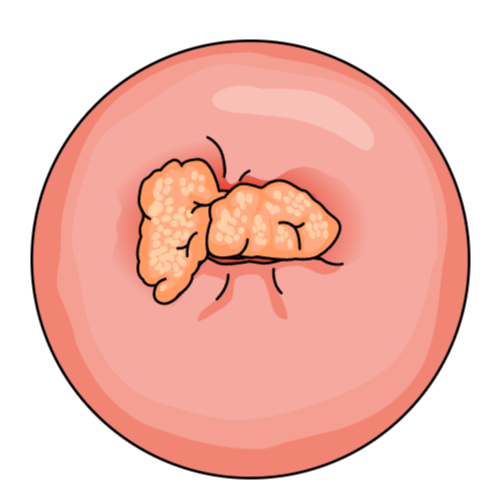
Cervical cancer is a form of cancer that develops in the cells of the cervix, which links the uterus to the vagina. Squamous cell carcinoma is the most prevalent kind of cervical cancer, accounting for 70% of cases, whereas adenocarcinoma is the least frequent, accounting for just 25%.
Adenocarcinoma is also the most difficult to diagnose since it begins higher in the cervix, making it harder to localize.
What causes cervical cancer?
Long-term infections with certain variations of human papillomavirus, also known as HPV, are the most prevalent cause of cervical cancer. HPV is a common virus that may be transmitted through sexual contact.
The human body relies on its immune system to stop viruses from causing harm, but in some individuals who have been exposed to HPV, the virus can live for many years, contributing to the process of normal cervical cells becoming cancer cells.
Despite the fact that HPV is the most common cause, there are some risk factors, such as smoking, passive smoking, having a weak immune system, and if your mother used diethylstilbestrol (DES) during pregnancy, a synthetic type of estrogen prescribed between 1939 and 1971 that has been linked to cancer, birth defects, and other developmental abnormalities.
Simplify the understanding of cervical cancer
A well-built infographic is the best choice for it. After all, with the perfect balance between written content and scientifically accurate illustrations, even the most complex subject can be easily explained with ease. Meet Mind the Graph, the best infographic maker.
Symptoms of cervical cancer
Some of the symptoms that a person suffering from cervical cancer may encounter include:
- Intercourse pain;
- Intercourse followed by bleeding;
- Vaginal bleeding, between the regular periods or after menopause;
- Menstrual bleeding that is thicker or lasts longer than normal;
- Pelvic ache;
- Change in the vaginal behavior, more discharge, or a strong or odd color or smell.
Diagnosis of cervical cancer
Cervical cancer is diagnosed using the following procedures:
Screening
Screening tests can aid in the detection of cervical cancer and precancerous cells that may develop into cervical cancer in the future. Screening entails:
- HPV DNA Test: Examining cells obtained from the cervix, looking for probable infections with any of the HPV strains most likely to cause cervical cancer;
- Pap-test: This test includes scraping and brushing the cells of the cervix, which are then sent to a lab to be examined for abnormalities in cells, such as cancer cells and cells that exhibit alterations that raise the risk of cervical cancer.
Colposcopy
A colposcopy process comprises a healthcare professional using a speculum to open the vagina so that a clear view of the cervix may be obtained, as well as the application of a vinegar solution to aid the detection of abnormalities in the organ. Following that, a colposcope will be put near the vagina and a strong light will be used to examine the cervix attentively. A colposcopy is frequently followed by a biopsy.
Biopsy
A biopsy is a process in which a sample of tissue is extracted from the cervix and examined under a microscope by a pathologist to look for indications of cancer. There are several types of biopsy, as listed below:
- Endocervical curettage: A procedure that collects cells or tissue from the cervix canal using a tiny spoon-shaped instrument called a curette. This is a straightforward procedure that is normally performed in a doctor’s office;
- Punch biopsy: A method that employs a sharp and hollow instrument to remove a tiny, round piece of tissue. Several regions of the cervix may need to be examined for this procedure.
- Cone biopsy (conization): A surgical procedure that removes a bigger, cone-shaped portion of tissue from the cervix and cervix canal. This method can be used to detect cervical cancer as well as remove precancerous or early-stage cancer. Because this involves anesthesia, it is performed in a hospital.
- Loop electrosurgical excision procedure (LEEP): This method involves passing an electrical current via a tiny wire loop to remove tissue from the cervix. This treatment, like the Cone biopsy, can be used to diagnose cervical cancer, as well as to remove precancer or early-stage cancer. The treatment is easy, but a local anesthetic is required.
Staging
One of the key points for understanding cervical cancer is the stages. If you are diagnosed with cervical cancer, you will require more tests to determine the stage of cancer. The stage of cancer is an essential factor to consider while deciding on the best treatment. Exams for staging include:
- Examine your bladder and rectum visually.
- Imaging tests. X-rays, CT scans, MRIs, and positron emission tomography (PET) scans can assist your doctor to identify if your cancer has progressed throughout your cervix.
What are the treatments?
Every case is unique, therefore it requires much inquiry to establish the best strategy for treating cervical cancer. Patients must ensure that they have the right team for the job.
| Stage | Subtypes | Treatment |
|---|---|---|
| Early-stage | IA1 | Surgery, total hysterectomy, radical hysterectomy, and conization. |
| IA2, IB, IIA | Radiation with brachytherapy and radical hysterectomy with lymphadenectomy. Radical vaginal trachelectomy with pelvic lymph node dissection, for cancer equal to or smaller than 2cm, is usually effective for preserving fertility. Cisplatin-based chemotherapy with radiation for patients with risk of recurrence. | |
| Advanced-stage | IIB, III, IVA | Cisplatin-based chemotherapy with radiation. |
| Metastatic-stage | IVB and recurrent cancer | Palliative treatments and chemotherapy using the medicine for disseminated cancer. |
HPV vaccination
After scientists started the process of understanding cervical cancer, an HPV vaccination became available for the particular kinds of HPV that cause nearly all cervical cancers. Gardasil 9 is the vaccination, and it protects against nine types of HPV, which are responsible for 90% of cervical cancer cases. HPV vaccine is advised for immunization at the age of 11 or 12 years, and everyone up to the age of 26 years should have the HPV vaccine if they have not already been properly immunized. However, HPV vaccination is not advised for anybody above the age of 26.
Because the vaccine is not available to everyone, frequent screening is advised. And, of course, even if you get the vaccine, you should still undergo frequent screening tests, your first screening should be at the age of 25 and then every five years after that.
Simplify and spread visual scientific communication across the globe
It is simple to disseminate information when employing highly understood graphic assets. Using the Mind The Graph tool, you can create stunning scientific, academic, and educational infographics and presentations in a few easy steps.

Subscribe to our newsletter
Exclusive high quality content about effective visual
communication in science.