Vaccines have long been a foundation of public health, protecting individuals and communities from infectious diseases. However, traditional vaccine development and delivery methods can be slow, expensive, and have limitations in their efficacy against certain pathogens. In recent years, researchers have been developing innovative technologies and approaches to enhance the effectiveness, safety, and speed of vaccine development and delivery.
What is the Importance of developing new vaccine technologies?
Developing new vaccine technologies is crucial for several reasons:
Addressing emerging and re-emerging infectious diseases: As new diseases continue to emerge and others re-emerge, there is a need for new and more effective vaccines to prevent and control their spread. Developing new vaccine technologies can help to address these challenges and provide faster, safer, and more effective ways to prevent and control infectious diseases.
Improving vaccine accessibility: Many traditional vaccines require refrigeration, making their distribution and storage in remote and low-resource areas challenging. Developing new vaccine technologies that do not require refrigeration can improve accessibility and help to ensure that individuals in remote and low-resource areas have access to life-saving vaccines.
Enhancing vaccine safety: Traditional vaccines are generally safe, but rare adverse events can occur. Developing new vaccine technologies that are safer and have fewer side effects can increase confidence in vaccines and help to address vaccine hesitancy.
Providing solutions for non-infectious diseases: Next-generation vaccines may have applications in non-infectious diseases such as cancer, allergies, and autoimmune disorders. Developing new vaccine technologies that can be used to prevent and treat these diseases has the potential to transform the field of medicine.
What are next-generation vaccines?
Next-generation vaccines refer to a new generation of vaccines that use innovative technologies and approaches to enhance the efficacy, safety, and speed of vaccine development and delivery. These vaccines aim to address the limitations of traditional vaccine platforms, which can be slow and expensive to produce, have limited efficacy against certain pathogens, and may require repeated booster doses.
Some examples of next-generation vaccine technologies include:
RNA vaccines
RNA vaccines are a type of next-generation vaccine that uses genetic material called messenger RNA (mRNA) to produce an immune response against a specific pathogen. RNA vaccines work by introducing mRNA into the body, which instructs cells to produce a viral protein that triggers an immune response. This immune response helps the body recognize and fight the pathogen in case of future exposure.
RNA vaccines have gained significant attention in recent years due to their use in the development of COVID-19 vaccines. The Pfizer-BioNTech and Moderna COVID-19 vaccines are both mRNA vaccines that have been shown to be highly effective in preventing COVID-19 infection.
Advantages of RNA vaccines include:
Rapid development: They can be designed and produced much faster than traditional vaccines, which require growing the pathogen in large quantities and inactivating or weakening it. This makes RNA vaccines an attractive option for addressing emerging infectious diseases.
Easy to customize: RNA vaccines can be easily customized to target different strains or variants of a pathogen by changing the genetic sequence of the mRNA.
Safety: RNA vaccines do not contain live or inactivated viruses, making them safe for people with weakened immune systems or allergies to certain vaccine components.
Efficiency: RNA vaccines can induce strong and specific immune responses, potentially providing better protection than traditional vaccines.
Viral vector vaccines
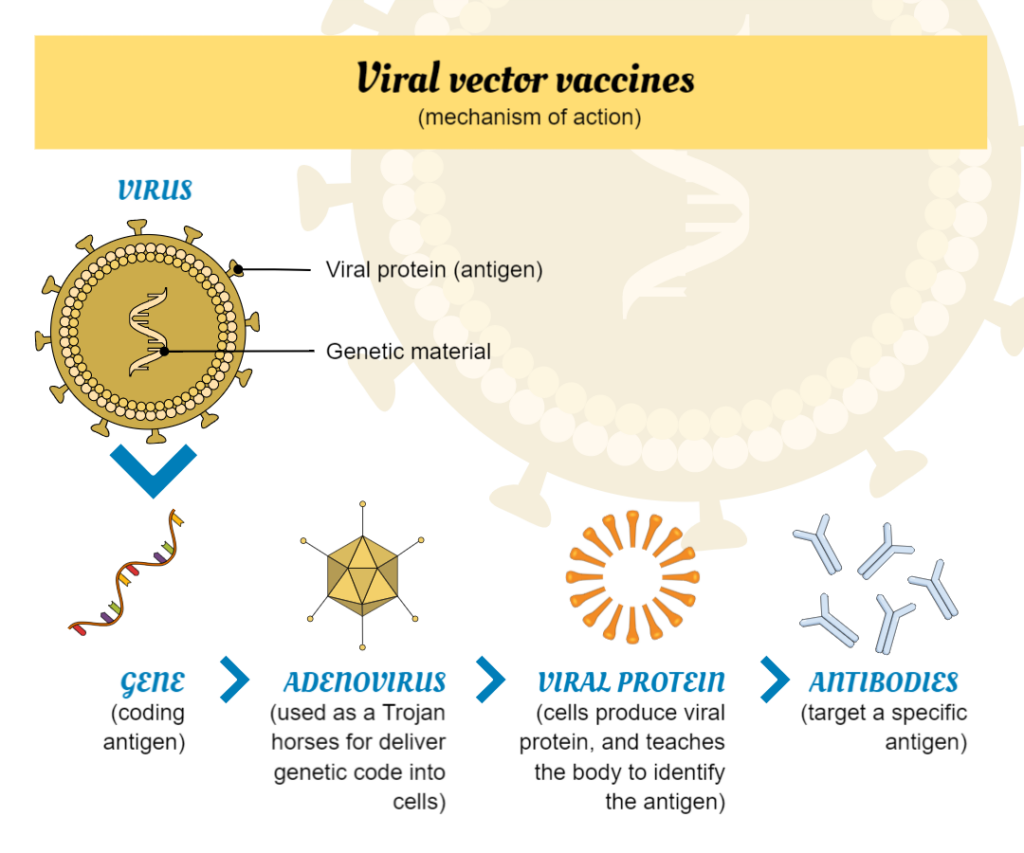
Viral vector vaccines are a type of vaccine that uses a virus to deliver genetic material into human cells. The virus used is typically a weakened or modified version of a different virus that does not cause disease in humans, but can still replicate within human cells. The genetic material that is delivered usually encodes for a specific antigen, which is a molecule that the immune system recognizes as foreign and produces an immune response against.
When a viral vector vaccine is administered, the virus enters human cells and releases the genetic material. The cells then use this genetic material to produce the antigen, which is presented on their surface. The immune system recognizes the antigen as foreign and mounts an immune response against it, producing antibodies and activating immune cells that can recognize and destroy cells infected.
Here are some examples of viral vector vaccines:
Johnson & Johnson COVID-19 vaccine: Uses a modified adenovirus as a vector to deliver a piece of genetic material from the SARS-CoV-2 virus that causes COVID-19 into cells.
AstraZeneca COVID-19 vaccine: Also uses a modified adenovirus as a vector to deliver genetic material from the SARS-CoV-2 virus. It is similar to the Johnson & Johnson vaccine but uses a different adenovirus vector.
Ebola vaccine: Uses a recombinant vesicular stomatitis virus (rVSV) as a vector to deliver a gene for the Ebola virus glycoprotein into cells.
Human papillomavirus (HPV) vaccine: Uses a modified virus called a virus-like particle (VLP) as a vector to deliver a piece of genetic material from HPV into cells.
DNA vaccines
DNA vaccines are a type of vaccine that uses a small piece of DNA to trigger an immune response in the body. The DNA used in these vaccines contains genetic instructions to produce specific antigens, which are proteins that are found on the surface of pathogens and trigger an immune response. When a DNA vaccine is injected into the body, the DNA enters the cells and instructs them to produce the antigen. The cells then display the antigen on their surface, which triggers an immune response.
DNA vaccines present some advantages when compared to more classical methods, especially in terms of speed of production, greater thermal stability at room temperature, and easy adaptation to new pathogens.
Here are some examples of DNA vaccines:
INO-4800 COVID-19 vaccine: Uses a small piece of DNA that encodes for the spike protein found on the surface of the SARS-CoV-2 virus that causes COVID-19. The vaccine is delivered into cells using a device that delivers electrical pulses to the skin.
VGX-3100 HPV vaccine: That uses a small piece of DNA that encodes for the antigens of the human papillomavirus (HPV), which is known to cause cervical cancer.
H5N1 influenza vaccine: Uses a small piece of DNA that encodes for the hemagglutinin protein found on the surface of the H5N1 influenza virus. The vaccine has been shown to be safe and immunogenic in clinical trials.
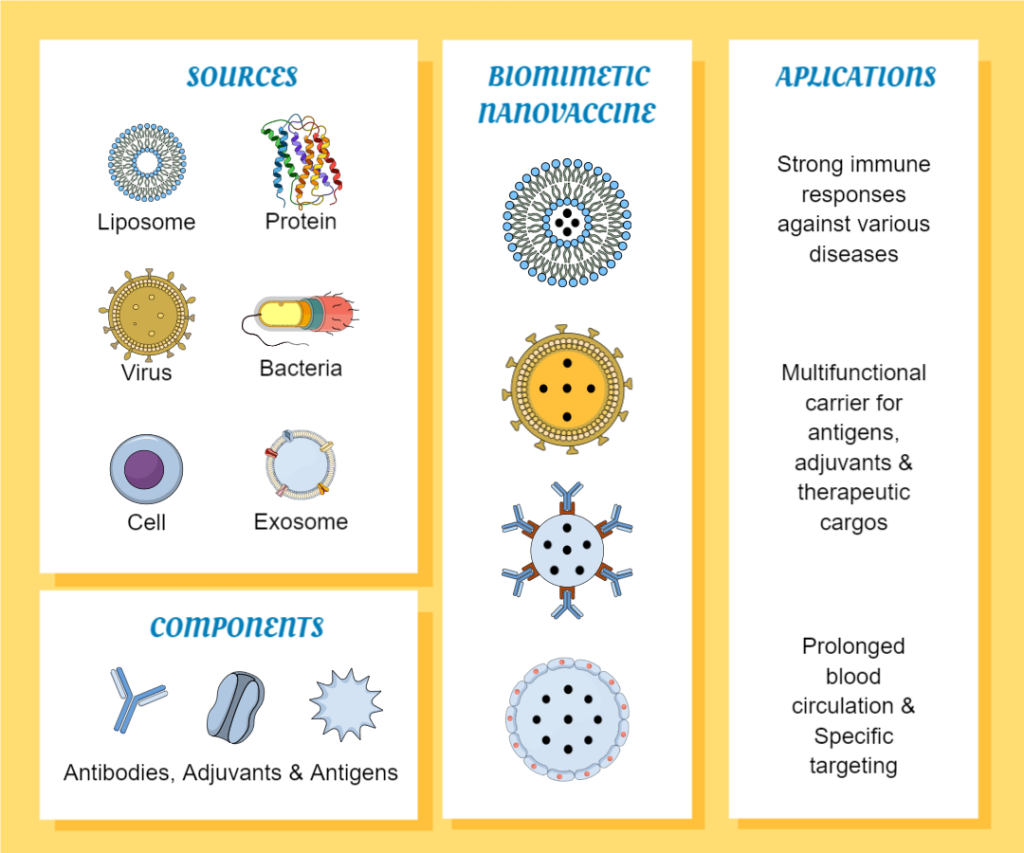
Nanoparticle vaccines
Nanoparticle vaccines are a type of vaccine that uses tiny particles to deliver antigens to the immune system. These particles can be made from a variety of materials, including lipids, proteins, and synthetic polymers, and are designed to mimic the size and structure of viruses or other pathogens.
When a nanoparticle vaccine is administered, the particles are taken up by immune cells, which then process the antigens and present them to other immune cells. This triggers an immune response, leading to the production of antibodies and activation of T cells that can recognize and destroy cells infected with the virus or bacteria that produce the antigen.
One advantage is their ability to mimic the size and structure of pathogens, which can enhance their ability to induce an immune response. Additionally, they can be designed to target specific cells or tissues, allowing for more targeted immune responses. They may also be more stable and have a longer shelf life than traditional vaccines, which can be important for distribution in low-resource settings.
Here are some examples of nanoparticle vaccines:
Moderna COVID-19 vaccine: This vaccine uses lipid nanoparticles to deliver mRNA that encodes for the spike protein of the SARS-CoV-2 virus.
Malaria vaccine: The RTS,S malaria vaccine uses nanoparticles made of a hepatitis B surface antigen and a portion of the malaria parasite to stimulate an immune response against malaria.
Influenza vaccine: The FluMist influenza vaccine uses live attenuated influenza virus particles as a nanoparticle vaccine to stimulate an immune response against influenza.
Next-generation vaccines have the potential to revolutionize the field of vaccinology, providing faster, safer, and more effective ways to prevent and control infectious diseases. They may also have applications in non-infectious diseases such as cancer, allergies, and autoimmune disorders. However, further research and development are needed to fully realize the potential of these new technologies.
Add visual impact to your posters with scientific illustrations
Mind the Graph is an online platform that offers scientists and researchers a library of scientifically accurate and visually impactful illustrations to enhance their posters, presentations, and publications. The platform provides a simple and intuitive interface that allows users to search for and customize the illustrations to fit their specific needs.

Subscribe to our newsletter
Exclusive high quality content about effective visual
communication in science.





