When discussing neurological disorders, few conditions emerge as both intricate and devastating as Amyotrophic Lateral Sclerosis, more commonly referred to as ALS. This enigmatic disease, often synonymous with Lou Gehrig’s disease in honor of the celebrated baseball player whose career was tragically affected by it, presents an intricate enigma that continues to captivate the attention of medical researchers, clinicians, and the wider public.
While ALS might not command the same widespread recognition as certain other neurological disorders, its impact on both those directly affected and their loved ones is profound, frequently accompanied by heartrending emotions. This article, titled “What is Amyotrophic Lateral Sclerosis and Its Effects?,” delves into the core of this tragic condition.
Sadly, the recent loss of Bryan Randall, a photographer and longtime partner of Sandra Bullock, has once again highlighted ALS in the public eye. Bryan’s passing at 57 emphasized the unforgiving character of the disease. Regrettably, ALS lacks a cure, and after diagnosis, individuals typically have an average life expectancy of 2 to 5 years.
What is Amyotrophic Lateral Sclerosis?
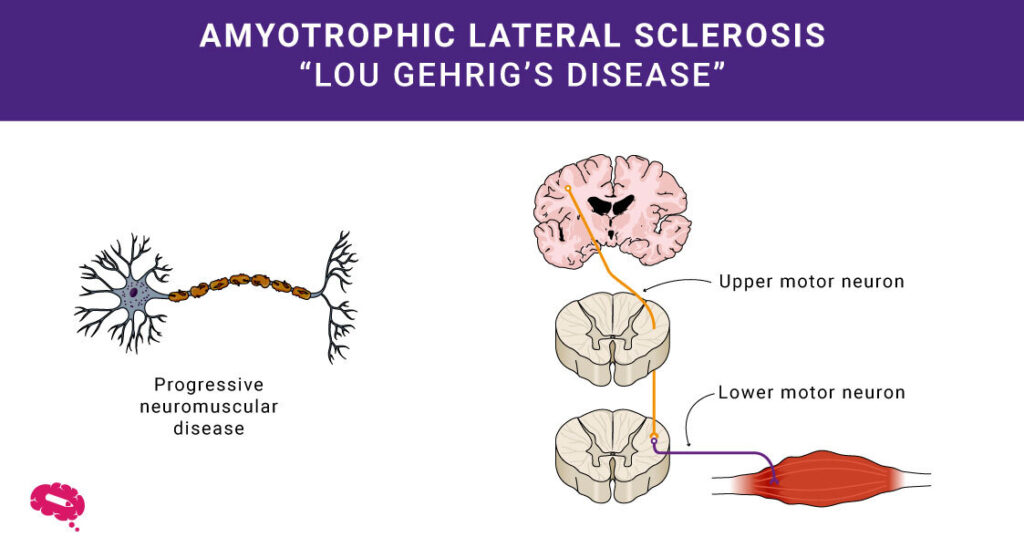
Medical science often uncovers complex mysteries in the realm of human health. One of them is Amyotrophic Lateral Sclerosis, or ALS. You might know it as Lou Gehrig’s disease. This condition affects the brain and spinal cord’s motor neurons, which control human muscles. In ALS, these neurons break down, making it hard to move muscles.
Definition of ALS
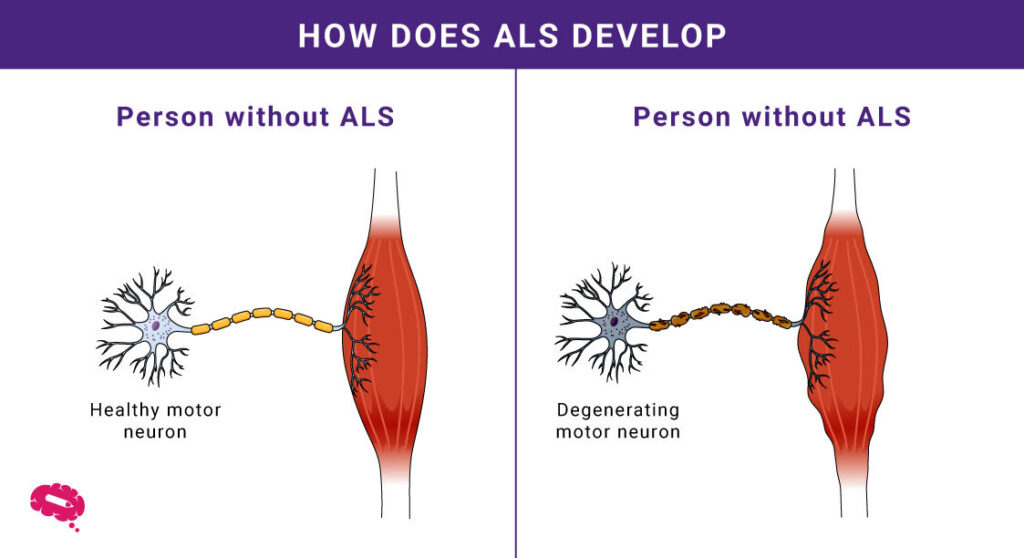
ALS, or Amyotrophic Lateral Sclerosis, is a disorder that affects how the human muscles work. This makes the human muscles get weaker over time, which can lead to problems with moving and doing everyday tasks.
Brief History and Background
The history of Amyotrophic Lateral Sclerosis (ALS) is a story of discovery that spans more than a century. It began in 1869 when French neurologist Jean-Martin Charcot first identified and described the disease. However, ALS gained wider recognition in 1939 when the legendary baseball player Lou Gehrig was diagnosed with it, leading to its colloquial name, “Lou Gehrig’s disease.”
Advancements in the 1960s and 1970s illuminated the disease’s core, revealing the progressive degeneration of motor neurons as its underlying mechanism. In the 1990s, genetic breakthroughs uncovered links between ALS and genes like SOD1 and TDP-43, deepening our understanding of its genetic components.
The 21st century marked significant milestones, including the viral Ice Bucket Challenge that raised both awareness and resources for ALS research. In 2016, the FDA approved the first ALS-specific drug, edaravone (Radicava), offering a novel approach to slowing disease progression.
As we navigate the 2020s, relentless research continues, exploring treatment possibilities, the genetic intricacies of ALS, and the underlying triggers. This journey underscores our dedication to unraveling the complexities of ALS and alleviating its impact on those affected.
Importance of Understanding ALS
Understanding ALS holds a significant role for various individuals, extending beyond medical experts to encompass society as a whole. The importance of this understanding stems from several key reasons:
Firstly, ALS does not discriminate based on demographics, making widespread comprehension crucial. Enhanced awareness of the disease equips medical professionals to identify it in its early stages, facilitating timely intervention and care for affected individuals.
Secondly, a deeper understanding of ALS serves as a wellspring of hope for families navigating its challenges. Clear insights into the disease’s progression and available treatments empower families to plan ahead, adapt their lives, and make informed choices.
Additionally, research efforts gain momentum through understanding. A robust grasp of ALS’s intricate nature accelerates the search for potential therapies and interventions. With enhanced understanding, resources can be directed more efficiently toward effective solutions.
Ultimately, understanding ALS rallies a collective front. Families, friends, caregivers, researchers, and the broader community unite to address this challenge. Through comprehensive understanding, a powerful movement against ALS is fostered, envisioning a future where ALS is synonymous with resilience, solidarity, and progress.
Understanding the Disease
Amyotrophic Lateral Sclerosis (ALS) is well-known for being a complex disease. Here are some crucial details to shed a light on:
Symptoms and Early Signs
Detecting ALS early relies on identifying its characteristic symptoms. Initial indicators frequently involve weakened muscles, especially in the limbs. Other potential signs encompass alterations in speech, muscle twitches, and feelings of fatigue.
Causes and Risk Factors
The exact cause of ALS is not fully understood, but it’s believed to be a result of a combination of genetic and environmental factors. Here are some of the known causes and risk factors associated with ALS:
- Genetic Factors: A small percentage (approximately 5-10%) of ALS cases are inherited, meaning they are caused by mutations in specific genes. The most well-known gene associated with familial ALS is the C9orf72 gene mutation. Mutations in other genes like SOD1, TARDBP, and FUS have also been linked to ALS. These genetic mutations can lead to the accumulation of abnormal proteins in neurons, causing damage and cell death.
- Environmental Factors: While genetic factors play a significant role in familial cases of ALS, environmental factors are also believed to contribute to the development of the disease. Exposure to certain toxins and chemicals, such as heavy metals, pesticides, and industrial pollutants, has been suggested as potential risk factors.
- Age: ALS typically develops in adults between the ages of 40 and 70, with the average age of onset being around 55-60 years. However, it can occur at any age.
- Gender: ALS is slightly more common in men than in women. The reasons for this gender difference are not fully understood.
- Race and Ethnicity: ALS occurs in all racial and ethnic groups, but it appears to be more common among Caucasians compared to other racial groups.
- Smoking: There is evidence to suggest that smoking might increase the risk of developing ALS. Smoking has been associated with oxidative stress and inflammation, which are thought to play a role in the progression of the disease.
- Physical Activity: There is some evidence that individuals with a history of high levels of physical activity may have a slightly increased risk of ALS. However, the relationship between physical activity and ALS risk is not fully understood and requires further research.
- Head Trauma: There have been suggestions that a history of traumatic head injuries might be associated with a slightly increased risk of ALS. However, the link between head trauma and ALS is still being studied.
How ALS Affects the Body
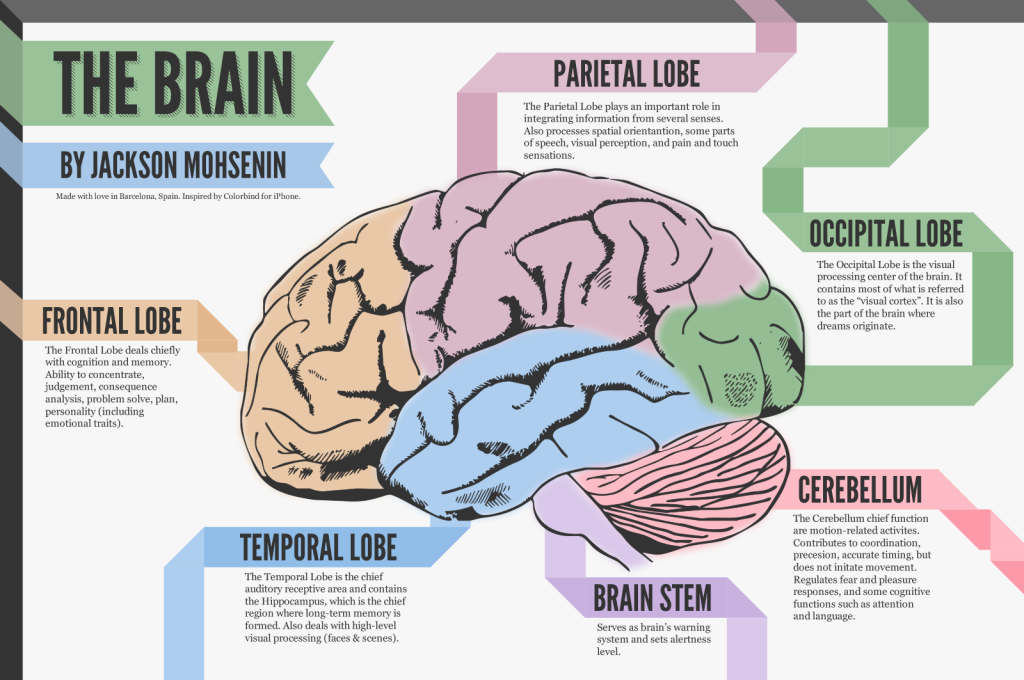
- Motor Neuron Degeneration: ALS targets motor neurons causing muscle weakness and loss of control.
- Muscle Weakness: Gradual degeneration leads to difficulty in movement and everyday tasks.
- Speech and Swallowing Issues: Muscles for speaking and swallowing are affected, causing slurring and difficulty eating.
- Breathing Problems: Respiratory muscles weaken, leading to breathing difficulties.
- Progressive Paralysis: Over time, increasing paralysis affects mobility and independence.
- Cognitive Changes: Some experience alterations in memory and decision-making, especially in ALS with frontotemporal dementia.
- Sensory Function Intact: Sensations like touch and sight usually remain unaffected.
- Life-Threatening Complications: Respiratory failure in advanced stages can be life-threatening.
Diagnosis and Testing
ALS diagnosis is a comprehensive process encompassing clinical evaluation, medical history assessment, neurological examination, and the exclusion of alternative conditions. It relies on a range of examinations, including electromyography (EMG), nerve conduction studies (NCS), and imaging, which collectively evaluate nerve and muscle function. Notably, ALS lacks a sole definitive test; rather, diagnosis hinges on the amalgamation of clinical observations and outcomes from various tests.
Diagnostic Procedures
- Medical history review to understand symptoms and their progression.
- Conducting a neurological assessment to evaluate muscle strength, reflexes, and coordination.
- Electromyography (EMG) measures muscle activity and detects nerve issues.
- Nerve conduction studies (NCS) assess nerve function and response.
Challenges in Diagnosis
- ALS symptoms overlap with other conditions, leading to misdiagnosis or delayed diagnosis.
- A lack of specific biomarkers can hinder early and accurate diagnosis.
- Progression and symptom variation make diagnosis challenging.
Differentiating ALS from Other Diseases
Unlike multiple sclerosis (MS), which primarily affects the central nervous system’s myelin sheath, ALS targets motor neurons responsible for voluntary muscle control.
While primary lateral sclerosis (PLS) shares certain characteristics with ALS, it predominantly involves upper motor neurons, distinct from ALS’s combined upper and lower motor neuron involvement.
Additionally, distinguishing ALS from spinal muscular atrophy (SMA) is crucial due to their shared impact on motor neurons; however, SMA primarily affects lower motor neurons, unlike ALS. The ability to differentiate ALS from these diseases is essential for accurate diagnosis and tailored treatment strategies.
Treatment and Management
The treatment and management of ALS encompass a multifaceted approach. Available treatment options aim to alleviate symptoms, slow disease progression, and enhance the quality of life for individuals with ALS.
Available Treatment Options
- The main focus of ALS treatment is to address symptoms, enhance the quality of life, and decelerate the progression of the disease.
- Medications like riluzole and edaravone are approved to potentially extend survival and delay progression.
- Baclofen and other drugs can help manage muscle spasticity, while medications like anticholinergics address excessive saliva production.
- Assistive devices, such as non-invasive ventilators and feeding tubes, assist with breathing and nutrition as muscle function declines.
Managing Symptoms and Quality of Life
- Physical and occupational therapy aids in maintaining muscle strength, mobility, and independence.
- Speech therapy assists with communication and swallowing difficulties.
- Supportive therapies, like nutritional counseling, psychological counseling, and support groups, help address emotional and practical challenges.
- Palliative care and hospice services improve comfort and quality of life in advanced stages.
Ongoing Research and Future Therapies
- Researchers continue to investigate ALS’s underlying causes and potential treatment targets.
- Gene therapy aims to correct genetic mutations responsible for familial ALS.
- Stem cell research explores using stem cells to replace damaged motor neurons.
- Innovative approaches include targeting abnormal protein accumulation and inflammation in ALS-affected neurons.
- Developing biomarkers could aid in early diagnosis and tracking disease progression.
- The search for new therapeutic agents and strategies remains active to provide more effective treatments for ALS.
Impact on Daily Life
Living with ALS profoundly alters daily life due to the gradual loss of muscle function and motor control. Simple actions such as walking, picking up objects, and even speaking become increasingly difficult as the disease progresses. Tasks that were once taken for granted require substantial effort or may become impossible to perform independently. As the ability to move and communicate declines, individuals with ALS often require assistive devices and adaptive techniques to maintain a certain level of functionality and engagement in their daily routines.
Support for Patients and Families
Living with ALS demands a robust support network for both patients and their families. Patients require physical, emotional, and psychological support to navigate the challenges of the disease. This includes assistance with daily activities, managing medical needs, and addressing emotional well-being.
Families and caregivers play a crucial role in providing this support while seeking answers to the question “What is amyotrophic lateral sclerosis?” They too need resources to cope with the emotional strain and practical demands of caregiving. Support groups, counseling services, and educational resources can provide valuable assistance in managing the complexities of ALS.
Stories and Perspectives from Individuals with ALS
Personal stories and perspectives from individuals living with ALS offer unique insights into the journey of facing this progressive disease. These stories highlight the strength, courage, and resilience required to adapt to the changes and limitations that ALS imposes. They provide a platform for sharing experiences, challenges, and coping strategies. Sharing these narratives fosters a sense of community among those affected by ALS, inspiring hope and providing a sense of connection that can help individuals and families feel less isolated in their struggles.
Join Our Fast-Growing Community To Revolutionize Scientific Communication!
Discover how the Mind the Graph platform empowers scientists with a comprehensive toolkit for effective communication. By seamlessly integrating visuals, data, and information, Mind the Graph simplifies complex scientific concepts, making them accessible to both experts and the wider audience.

Subscribe to our newsletter
Exclusive high quality content about effective visual
communication in science.